Eligibility & Benefits Verification Features
Appointment Confirmation
- Confirm appointment one business day in advance.
- Conducted during normal business hours.
- Contact patient via phone and /or SMS.
- Update EMR/ PMS when patients reply.
- Reschedule appointment when necessary.
- Send personalized text messages as may be requested by practices.
Eligibility & Benefits Verification
Patient Demographic Validation
- Confirm eligibility and benefits three business days in advance.
- Obtain new or replacement insurance carrier from patient.
- Update EMR/ PMS with new insurance carrier information, policy, or both.
Coverage Validation
- Benefits Validation.
- Determine copays.
- Determine deductible (met or unmet).
- Determine coinsurance.
- Update billing software.
- Communicate to practice via EMR / scheduler notes.
- Advise reception of the actual amount to be collected from the patient at time of check-in. (i.e., past due balances plus any co-pays and deductibles.)
Miscellaneous
- EMR/ PMS ownership lies with the Practice.
- All additional third-party payments to be billed as per actual, such as clearing house charges, patient statement vendor, etc.
- Physician has access to a dedicated Account Manager at Billing Advisors (By Phone) 24 hours & 7 days a week.
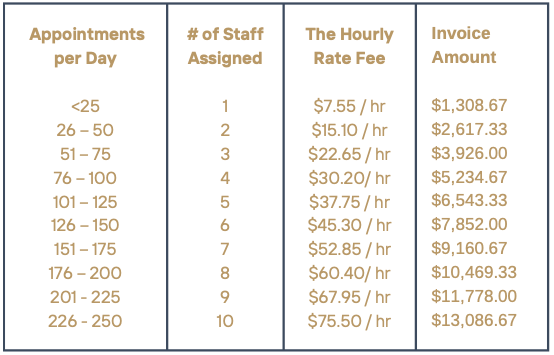
Pricing
The Fee for Service is pre-paid. It is based the average number of patients seen per day. The rate is then multiplied by the number of staff corresponding to the number of appointments then multiplied by an 8 hour day, then multiplied by a 5 day work week, then multiplied by 52 weeks in a year, then divided 12 months in a year. This will become the monthly amount due.
The invoice is issued on the 16th of each month. It is due upon receipt.