Billing & Coding Features
Appointment Confirmation
- Confirm appointment one business day in advance.
- Conducted during normal business hours.
- Contact patient via phone and /or SMS.
- Update EMR/ PMS when patients reply.
- Reschedule appointment when necessary.
- Send personalized text messages as may be requested by practices.
Eligibility & Benefits Verification
Patient Demographic Validation
- Confirm eligibility and benefits three business days in advance.
- Obtain new or replacement insurance carrier from patient.
- Update EMR/ PMS with new insurance carrier information, policy, or both.
Coverage Validation
- Benefits Validation.
- Determine copays.
- Determine deductible (met or unmet).
- Determine coinsurance.
- Update billing software.
- Communicate to practice via EMR / scheduler notes.
- Advise reception of the actual amount to be collected from the patient at time of check-in. (i.e., past due balances plus any co-pays and deductibles.)
Referral Management
- Identify patients requiring a referral.
- Advise PCP that a referral is required.
- FAX patient’s PCP for Referral Request providing all requisite details.
- Follow up online to obtain referral and download and update EMR.
- Follow up with the PCP referral department in case a referral is not obtained to ensure referral is in place before DOS.
- Collect procedure, Dx codes and location details from Practice via EMR.
Prior Authorizations
- Identify patients requiring a prior authorization.
- Advise PCP that a referral is required.
- FAX patient’s PCP for Referral Request providing all requisite details.
- Follow up online to obtain referral and download and update EMR.
- Follow up with the PCP referral department in case a referral is not obtained to ensure referral is in place before DOS.
- Collect procedure, Dx codes and location details from Practice via EMR.
Medical Billing
Charge Posting
- CPT and ICD (Coded by the Practice).
- Modifiers – Adding them where relevant.
- Adding Authorization numbers to charges.
- Copay posting to the correct line.
- NCD/ LCD (Ensuring CPT to ICD compatibility).
- NCCI.
- Claims Transmission.
Claim Scrubbing (Level I and II)
- Resolve and refile rejected claims within 48 hours.
Secondary Claims Management
Clearing House Follow Up & Other Troubleshooting
- Call and resolve any sort of issues with the clearing house.
- Call and resolve any sort of issues with the EMR/ PMR.
Payments Posting
- EOBs posting - (Explanation of Benefits).
- ERAs processing - (Electronic Remittance Advice).
Patient Funds Posting
- Post all patient funds to the appropriate line items.
Refunds Processing
- Process all insurance refunds and recoupments.
- Process all patient refunds for overpayments.
Patient Statements Management
- Run statements report, once monthly.
- Review all statements for accuracy before sending out.
A/R Recovery Management
- Current insurance A/ R recovery.
- Current patient A/ R recovery by making soft patient collection calls.
- Old Insurance A/ R recovery.
- Old patient A/ R recovery by making soft patient collection calls.
Fee Schedule Management
- Perform annual Fee Schedule updates in consultation with practice.
Credentialing
- Assessing legal and structural setup.
- Securing a Type 2 NPI (if applicable).
- Obtaining an EIN for new entities.
- Registering new locations with CAQH.
- Ensuring malpractice insurance compliance.
- Coordinating credentialing with commercial payers (BCBS, Aetna, UHC, etc.).
- Managing Medicare enrollment via PECOS.
- Processing Medicaid applications (state-specific).
- Setting up clearinghouse integration and billing systems.
To support these activities, we maintain comprehensive logs for key applications and processes—such as NPI registration through NPPES, EIN issuance via the IRS, and CAQH profile management. We also handle all documentation and attestations, coordinate with insurance carriers for new or updated credentialing applications, manage location-specific malpractice policies, and ensure proper enrollment and claims routing through EFT/ERA setups.
View ComparisonMiscellaneous
- EMR/ PMS ownership lies with the Practice.
- All additional third-party payments to be billed as per actual, such as clearing house charges, patient statement vendor, etc.
- Physician has access to a dedicated Account Manager at Billing Advisors (By Phone) 24 hours & 7 days a week.
Pricing
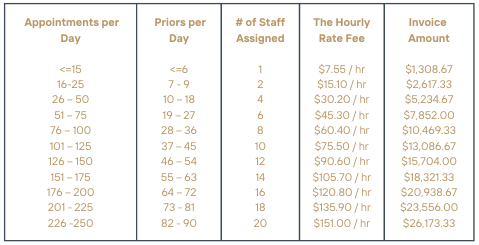
The Fee for Service is pre-paid. It is based the average number of patients seen and not to exceed the maximum number of authorizations allowed per day. The rate is then multiplied by the number of staff corresponding to the number of appointments then multiplied by an 8 hour day, then multiplied by a 5 day work week, then multiplied by 52 weeks in a year, then divided 12 months in a year. This will become the monthly amount due.
The invoice is issued on the 15th of each month. It is due upon receipt.
Disclaimers
Client will authorize BA to prepare, process and submit claims to commercial and government payors. BA will apply its best efforts to obtain reimbursement for Client’s charges for all clinical procedures and medical services provided to patients. All such claims shall be submitted by BA in the Client’s name and utilize provider numbers assigned to the Client by the respective insurance payor. Claims will be submitted by electronic, facsimile, or paper means. Payment of all claims filed on behalf of Client shall be directed to such accounts to which Client has control. BA shall post payments received from the insurance companies to the patient's record.
It is the responsibility of the Client to contact the patient directly, when necessary, to secure full payment for the Client. Client is the only party to this Agreement to negotiate a repayment plan with patients.
Client will authorize BA to medically code any services performed by client for which a superbill is not used. This can be for services performed at a facility other than the Client’s office (i.e., hospital, clinic, other practices, etc.) The coding fee is $2.00 per chart.
Credentialing process typically takes 30 to 180 days to complete, covering federal, state, and private health insurance payers. To ensure a seamless and timely credentialing experience for new physicians, we assign dedicated resources who manage the process with precision and attention to detail. For this we charge a fee of $300 per new hire. For existing physicians we maintain the credentialing requirements for all physicians as a part of our service.
BA will be responsible for the collection of claims and submissions both after and before the effective date of this contract. For claims, whose date of service, is posted after the effective date there is no fee on collected funds. For claims, whose date of service, is posted before the effective date the fee on collected funds shall be 15%. For claims posted before the effective date, BA will review each outstanding claim and assess whether it should be written off, needs to be resubmitted, or any other actions that would work towards the collection on such claims.
