Prior Authorization Features
Appointment Confirmation
- Confirm appointment one business day in advance.
- Conducted during normal business hours.
- Contact patient via phone and /or SMS.
- Update EMR/ PMS when patients reply.
- Reschedule appointment when necessary.
- Send personalized text messages as may be requested by practices.
Eligibility & Benefits Verification
Patient Demographic Validation
- Confirm eligibility and benefits three business days in advance.
- Obtain new or replacement insurance carrier from patient.
- Update EMR/ PMS with new insurance carrier information, policy, or both.
Coverage Validation
- Benefits Validation.
- Determine copays.
- Determine deductible (met or unmet).
- Determine coinsurance.
- Update billing software.
- Communicate to practice via EMR / scheduler notes.
- Advise reception of the actual amount to be collected from the patient at time of check-in. (i.e., past due balances plus any co-pays and deductibles.)
Referral Management
- Identify patients requiring a referral.
- Advise PCP that a referral is required.
- FAX patient’s PCP for Referral Request providing all requisite details.
- Follow up online to obtain referral and download and update EMR.
- Follow up with the PCP referral department in case a referral is not obtained to ensure referral is in place before DOS.
- Collect procedure, Dx codes and location details from Practice via EMR.
Prior Authorizations
- Identify patients requiring a prior authorization.
- Advise PCP that a referral is required.
- FAX patient’s PCP for Referral Request providing all requisite details.
- Follow up online to obtain referral and download and update EMR.
- Follow up with the PCP referral department in case a referral is not obtained to ensure referral is in place before DOS.
- Collect procedure, Dx codes and location details from Practice via EMR.
Miscellaneous
- EMR/ PMS ownership lies with the Practice.
- All additional third-party payments to be billed as per actual, such as clearing house charges, patient statement vendor, etc.
- Physician has access to a dedicated Account Manager at Billing Advisors (By Phone) 24 hours & 7 days a week.
Pricing
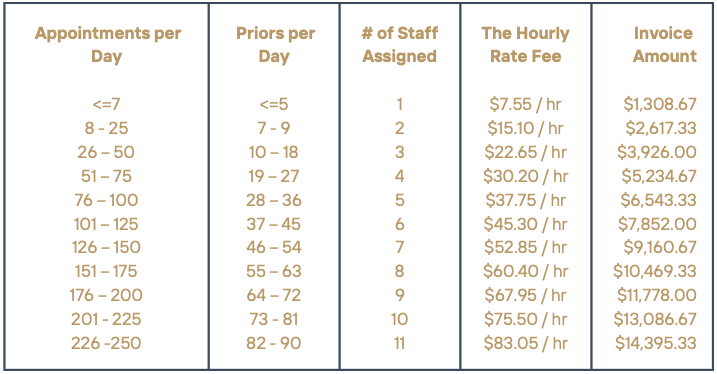
The Fee for Service is pre-paid. It is based the average number of patients seen and not to exceed the maximum number of authorizations allowed per day. The rate is then multiplied by the number of staff corresponding to the number of appointments then multiplied by an 8 hour day, then multiplied by a 5 day work week, then multiplied by 52 weeks in a year, then divided 12 months in a year. This will become the monthly amount due.
The invoice is issued on the 16th of each month. It is due upon receipt.